Disclaimer — This is about Severe Autism, not higher-functioning autism or Asperger’s Syndrome. Individuals with those types of autism often do their own writing about their worlds, which are usually extremely different — severely different — from that of Severe Autism.
~~~
After twenty seven years of severe autism in our family, we still don’t know exactly what it is, how it’s caused, or how to effectively “fix” it.
And so this is what too many families like ours, with severe autism, still go through, with no end in sight.
~~~
Ben was on his bedroom floor. He could not get up. When his staff tried to help the 6’2” 250-pound guy get out of bed, he slid to the floor. An ambulance took him to the nearest Emergency Room, where four of his staff were waiting. And Emergency Rooms + Ben can be a bad mix.
As usual, the ER was packed. He was there all day, and transferred to a room in the middle of the night, continuing an ordeal that had begun the week before with worsening limping, and didn’t end for another 12 days.
We have autism to blame, 100%, for the ordeal, but not for the problem that put Ben in the hospital in the first place.
And this is one of the nastiest hallmark’s of severe autism — communication. Or the lack of it.
We had no idea what the problem was, or what was causing it. None.
There were theories. But all Ben could “tell” us — behaviorally — was that he was hurting. Karen drew and labeled a human body, trying to get Ben to point to the pain. “Ben, where does it hurt?” He pointed to an ear. His ear was fine.
Ben has never been any good at telling us when or where something hurts. When he was in his early teens, I saw him look at his arm with a furrowed brow, before I noticed he was being stung by a bee. He flicked it off, and went back to what he was doing. The bee sting left a red, quarter-sized welt. Ben never showed any reaction.
And how about this doozie: A few years ago, Ben had a routine dental appointment for a cleaning and check-up — in a hospital operating room, with seven men holding him down as he fought to avoid the gas mask to put him out so he could have his check-up.
When the dentist got into his mouth, she saw something that still fills me with horror.
One of Ben’s back molars was gone, leaving only a few shards of shattered tooth. He’d never shown any signs of mouth pain. Can you imagine what he went through?
The dentist cleaned it out. Ben awoke with no signs of discomfort. He was ready for McDonald’s.
So here we were, again. Ben seemed fine until he started limping the week before, and it got worse quickly. I’m pretty sure, knowing Ben, that he had been in pain before there were any outward signs.
Now hospitalized, Ben had X-rays. Zilch. CAT scan. Zilch again.
And now the biggest terror we were facing was talk of skilled nursing. The idea was, once they figured out what was wrong, and if it were problems with ligaments or tendons, which Ben has a history of in his other leg, he would be discharged to a facility for rehab.
What?!? WHAT?!?!?!?!?!?!?!?!?!?!!!!!!!!!!!!!!
No freaking way. Beyond the absurdity and impossibility of him complying with the demands of rehab, Ben in a skilled nursing facility would require round-the-clock staffing, which is not something his provider would be able to manage.
This was becoming more unthinkable by the minute. And we still didn’t know what was wrong.
It was time for Ben’s MRI. But the first attempt failed because, hey this is Ben, Ativan wasn’t enough to mellow him out, and he wouldn’t lie down. Being the weekend, this delayed things for two days, because he had to go under general anesthetic for the MRI.
But it was worth the wait. It wasn’t his foot. It wasn’t his leg, or ligaments, or his tendons.
It was his spine.
Ben would need back surgery for a “significantly” herniated disc.
We almost passed out. Back surgery? For our Benny Boy??? We could NOT believe it. We immediately called his primary care doc for a second opinion. He agreed.
But as we got more information, our shock turned into relief.
As back surgeries go, this isn’t a “bad” one. In fact, it’s the easiest back surgery you can get. Assuming there was nothing else going on, Ben should be able to walk right away, with pain lasting only 3 to 5 days. In fact, this surgery is typically done (but not for Ben) as an out-patient procedure. Ben wouldn’t need a skilled nursing facility after all!
We don’t know how the skilled nursing idea would have panned out anyway. The hospital staff in charge of finding a place for Ben to go for rehab could not find a place to take him, given his very special needs. We stopped hearing from them even before the diagnosis was made.
It was reminiscent of how Ben, and Karen and I, ended up lifetime residents of Ohio. When he aged out of school district funding at 22, nobody, literally, in Illinois would offer him a spot in a group home. They couldn’t, or wouldn’t, be able to handle him.
So what would have been a relatively simple problem for you or me — a backache solved by a doctor’s visit and a day in the hospital — became weeks of fear and pain and anxiety and sleuthing and a dozen nights in a hospital bed.
But Ben is luckier than most. Through all of this, he was surrounded by dedicated, extremely caring, and very worried staff. Ben had someone with him around the clock in his hospital room that he knew and liked, if not loved. This included staff who currently work with him in his house and his day program; people who used to work with him in the cottage and at his school when he was younger; and folks in administration — bosses! — who were staff in Ben’s olden days a decade ago, pulling all-nighters. Never have we been more grateful for Ben to be where he is.
But you are probably wondering how Ben survived this ordeal.
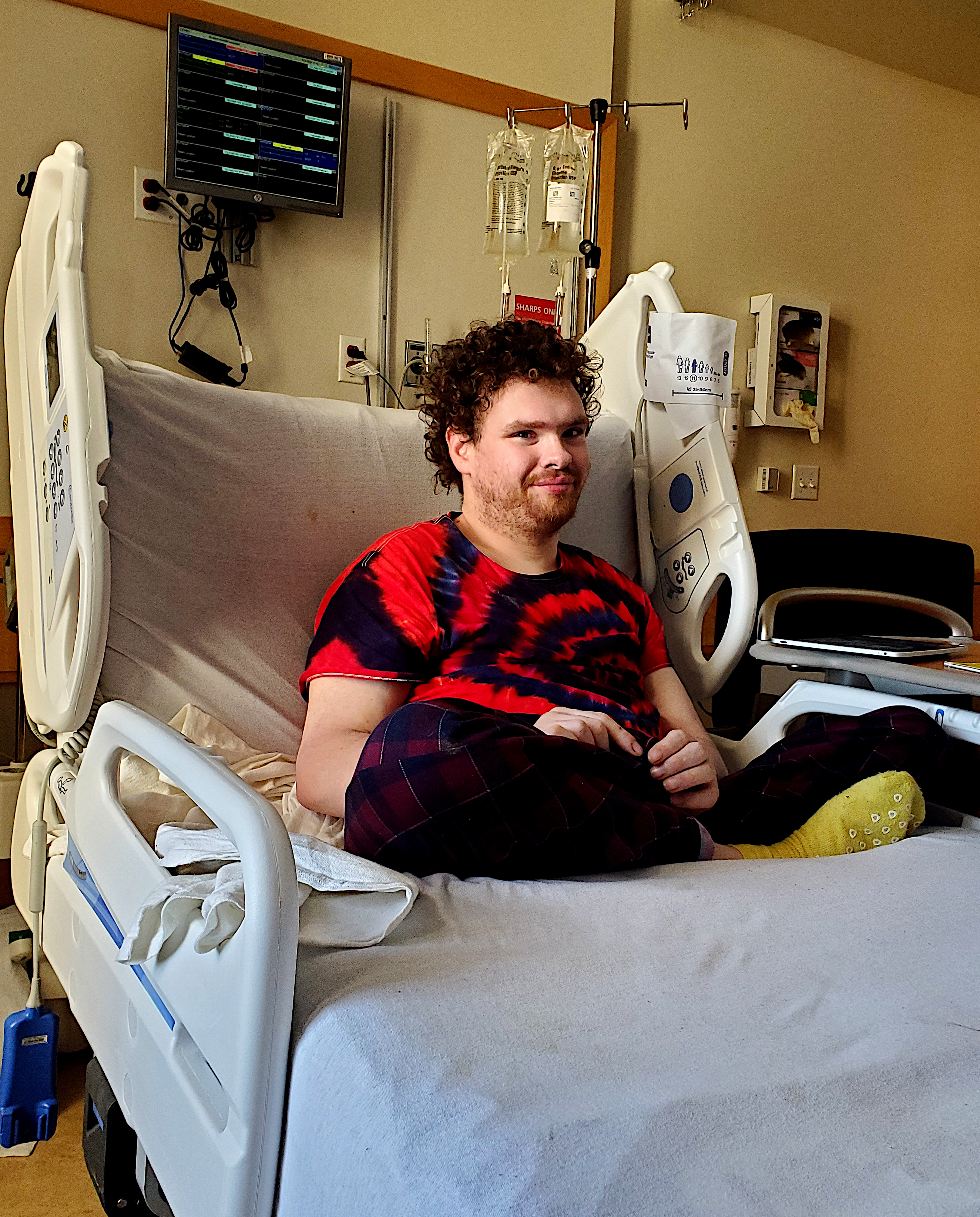
He LOVED it! Calmly lying or sitting cross-legged in his bed, Ben might’ve known, on some level, that people were responding to his pain, and that he didn’t have to walk any more.
And it was probably one of his favorite times of his entire life.
Think about it:
He likely wasn’t feeling any pain in bed;
He had no demands placed on him;
He loves doctors, especially when they use their stethoscopes;
He had a big box of books;
He had his iPad with all his music;
He had a TV in his room showing Disney movies he loves;
In other words: Club Med Hospital Bed!
And I learned that Ben listens to music on his own, with his iPad. I felt like I was looking back in time 50 years, at myself, sitting cross-legged (like Ben), staring at an album cover (Ben’s iPad), and fully concentrating on the music. Over a couple of hours, Ben cycled through bluegrass, jazz, kid songs, holiday songs, and Beethoven 7th symphony — all four movements.
And another shock, in a good way, was how University Hospitals treated him and us. As anyone who’s been hospitalized knows, they, and the insurance companies, want to get you out ASAP, if not sooner. And UH acted very un-hospital-like.
Maybe it was because they grasped how atypical our situation was, which might not have been the case two decades ago, before Autism Awareness. When we were talking to the doctor about Ben and his recovery, he could tell we were worried about him going home right after surgery.
He said, “We’re not kicking you out.”
So Ben had his “outpatient” surgery on a Thursday. He was a little shaky but was up and around that evening. And they didn’t discharge Ben until the following Tuesday, when he was almost as good as new, and ready to return to his house.
And boy, was he ready. Earlier, when I’d talked with him about going home and going back to MAAP, his day program, he said “No MAAP!” He was very happy hanging in the hospital.
The day before discharge, he told me, emphatically, “Go to MAAP!”
Another big surprise for us was Ben’s housemates. They all came up to say “Hi!” when he got back to the house. They actually missed him! We were not expecting this. When you see his house in action, the guys don’t seem particularly interested in each other. The staff are the ones who do things for and with them. But the guys clearly know who’s who, and they are attached in their own autistic ways. Or as one of his staff said, “They’re family.”
As for us, it’ll take a while to get beyond this, emotionally. One of the nightmares for parents of people like Ben is, what happens when he gets seriously ill, or injured, or is in pain?
These are not worries that diminish. Quite the opposite. Being autistic doesn’t make you immune to the usual ravages of time on our bodies. The problems of communication become more and more acute, and dangerous, the older they get. It is no mystery why people suffering with severe autism on average have much shorter life spans.
And it is no mystery why parents dealing with severe autism suffer from PTSD.
But though I would never wish the past few weeks on my worst enemy (well, there was this one jerkwad in high school, but anyway), at least Ben had a great time. The first time he saw us after he was discharged, he told Karen:
“Hospital.”
We think he was reminiscing.
~~~
Karen’s social story for our first visit with the big guy, post-crisis:
Ben’s back was hurting.
It was hurting when Ben was walking.
Ben went to the hospital.
The doctor gave Ben some tests.
The doctor said Ben needs an operation!
Ben had an operation on his back.
Now Ben can walk again.
And in the category of, “The more things change, the more they stay the same,” these are a few things I’ve written in previous Autism Awareness months:
World Autism Awareness Day with Ben Royko
Maybe Next Year (World Autism Awareness Day 2019)